Medically reviewed by Rami Allan, ND
In the intricate web of health factors, there’s one amino acid that’s been quietly making waves—homocysteine. Although it might not be a household name, its impact on well-being is significant. In this blog, we’ll provide a brief overview of what homocysteine is, why it matters for achieving peak health, and how maintaining proper methylation plays a vital role in keeping homocysteine levels in check.
What is Homocysteine?
Homocysteine is an amino acid that naturally occurs in the body as part of the process of breaking down proteins, especially the amino acid methionine. Methionine is essential for various bodily functions, and as it gets broken down, it gives rise to homocysteine. A certain level of homocysteine is normal and necessary for the body’s processes—an optimal range is between 5 and 8 micromoles per liter—but elevated levels in the blood can cause health concerns. While there is no consensus about the upper reference limits for plasma homocysteine concentrations, most research indicates that a plasma homocysteine level less than 10 micromoles per liter is associated with a lower risk of cardiovascular dysfunction, with substantial risk for coronary artery issues occurring between 10 and 15 micromoles per liter.
An increasing number of studies have been published that show elevated homocysteine levels to be a predictor of potential health problems. Raised plasma homocysteine concentrations both predict and precede the development of cardiovascular health conditions. Additionally, elevated homocysteine levels have been linked to a range of other health issues, including autoimmune conditions, declining memory, osteoporosis, thyroid issues, migraines, low mood, fatigue and more.
Factors Contributing to Elevated Homocysteine
Let’s look at some factors in the mix that can affect homocysteine levels.
- Genetics: Some people are more predisposed to higher homocysteine levels due to their genetic makeup, which can affect how efficiently their body processes and clears homocysteine. It is estimated that over 50% of the US population has genetic enzyme deficiencies that make it difficult for them to convert folic acid into its usable 5-MTHF form, potentially causing impaired homocysteine metabolism.
- Nutrition: B vitamins—B6, B12, and folic acid—are the unsung heroes here. They are crucial for the proper metabolism of homocysteine. Foods rich in B vitamins include leafy greens, legumes, nuts, and lean meats. A diet lacking in any of these B vitamins, or depletion of B vitamins caused by certain medications, can lead to elevated homocysteine levels in the blood.
- Lifestyle Factors: Smoking, excessive alcohol consumption, chronic stress, toxin exposure, certain prescription drugs, and a sedentary lifestyle can all contribute to imbalanced homocysteine levels.
The Role of Methylation
Methylation is a complex biochemical process that involves adding a “methyl group” to various molecules like DNA, proteins and neurotransmitters in the body. This methyl tag acts as a sort of switch, turning genes on or off, influencing how proteins are made, and even affecting how messages are transmitted in the brain. More than 200 of the body’s vital functions rely on methylation, such as digestion, regulating gene expression, repairing DNA, detoxification, neurotransmitter synthesis, skin repair and energy production.
Let’s explore how methylation works with an example, using a musical analogy.
Imagine the body’s DNA is like a big sheet of music, and the genes are individual musical notes. These notes come together to create different melodies, just like genes come together to build different parts of the body.
Now, think of methylation as tiny musical symbols that are added to the sheet music. These symbols can change the way the music sounds.
Let’s say you’re playing a song on the piano, and there’s a part where the music says to play a note really loud. But you decide that it would sound better if that note was a bit softer. So, you add a little mark next to that note that tells you to play it more gently. This mark changes how that part of the music sounds.
In the body, methylation is like those marks on the sheet music. Methyl groups are added to specific parts of the DNA, and they can change how certain genes “sound” or function. They can make some genes more active, like turning up the volume on certain musical notes, and they can make other genes less active, like playing some notes more softly.
For instance, if the body needs more of a certain protein, methylation can make that gene louder, increasing its activity. On the other hand, if the body doesn’t need a specific protein at the moment, methylation can make that gene quieter, reducing its activity.
Just like adding marks to sheet music can transform the way a song is played, methylation adds these molecular marks to DNA to fine-tune how the body functions. It’s a way for the body to create its unique “music” and adjust its responses to different situations.
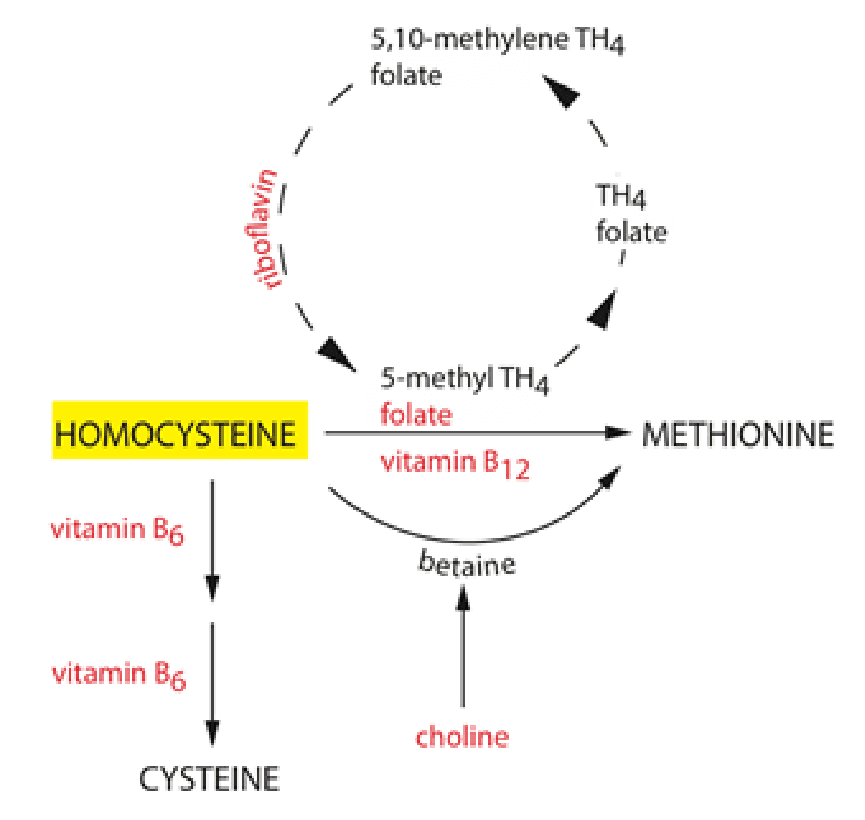
In the context of homocysteine, methylation plays a crucial role in converting homocysteine into other substances that are less harmful. When methylation is working optimally, it helps keep homocysteine levels within a healthy range, minimizing the risk of health problems.
Methylation relies on those essential B vitamins mentioned earlier—B6, B12, and folic acid. These vitamins act as co-factors or “methyl donors”, helping the body carry out the methylation process effectively. Activated forms of these nutrients are the best options to ensure healthy methyl pathways. When homocysteine interacts with the B vitamins, it converts into two substances:
- Methionine, an essential amino acid and antioxidant that creates proteins; and
- Cysteine, a nonessential amino acid created from methionine that reduces inflammation, increases communication between immune cells and promotes liver health.
Additional methyl donors that participate in methylation and nutrients that support methylation include:
- Betaine (Trimethylglycine)
- Choline
- Zinc
- Magnesium
- Sulfur-Containing Amino Acids
- Antioxidants
- Omega-3 Fatty Acids
If you suspect that high homocysteine levels may be an issue for patients, labs can provide their vitamin B levels, and serum homocysteine and methylation panel testing provide additional baseline measurements. Methylation genetic testing can give you more insight into why homocysteine levels might be higher than normal. The more gene polymorphisms, the more susceptible your patients will be to methylation issues.
High levels can, in many cases, be normalized through diet and vitamin supplementation. The key nutrients that help lower homocysteine levels are folate, the vitamins B12, B6 and B2, zinc and betaine [trimethylglycine (TMG)].
References
Brosnan JT, Jacobs RL, Stead LM, Brosnan ME. Methylation demand: a key determinant of homocysteine metabolism. Acta Biochim Pol. 2004;51(2):405-13.
“High Homocysteine.” Linus Pauling Institute, 9 Aug. 2022, lpi.oregonstate.edu/mic/health-disease/high-homocysteine.
Peng HY, Man CF, Xu J, Fan Y. Elevated homocysteine levels and risk of cardiovascular and all-cause mortality: a meta-analysis of prospective studies. J Zhejiang Univ Sci B. 2015 Jan;16(1):78-86.

