As formulas emerge that feature cannabinoids beyond CBD, it has become challenging to match up the different cannabinoid formulations with their potential indications. One such phytochemical, cannabidiolic acid (CBDa), is the focus of this blog. Read on to learn about CBDa — its relationship to CBD (cannabidiol) and the hemp plant, along with its most promising clinical applications.
What exactly is CBDa?
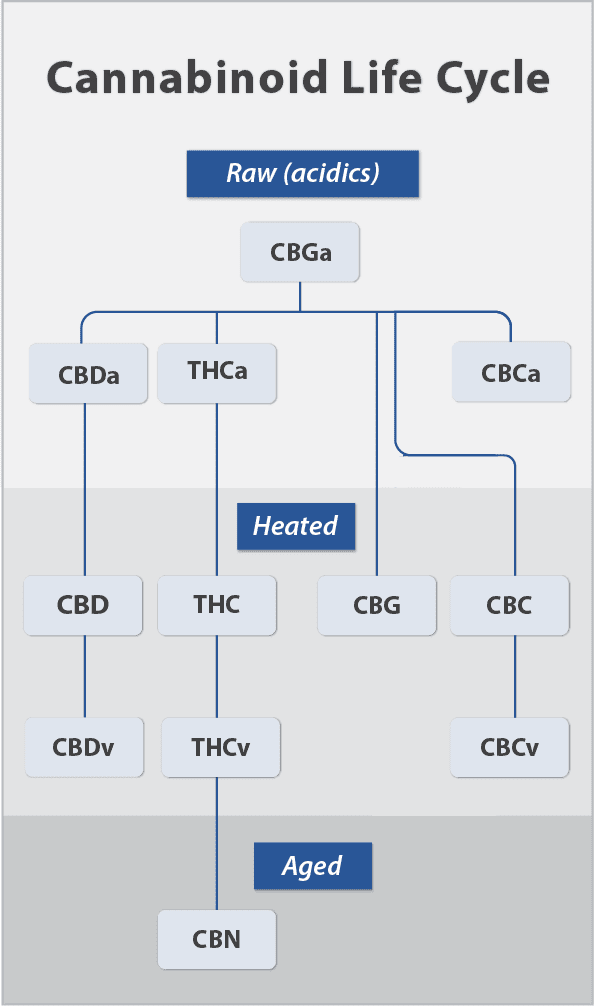
CBDa is a naturally occurring compound found in the hemp plant that is often overlooked in favor of its more well-known derivative, CBD. CBDa is the precursor to CBD, meaning that it is the acidic form of CBD, present in the cannabis plant in its natural or “raw” form before it is decarboxylated (heated) and converted into CBD. This process occurs naturally over time or through heating, such as during the extraction process. When heat is introduced, the carbon dioxide and hydrogen acidic part of the molecule are removed, creating a new molecular structure.
Initially, CBDa was dismissed as having little to no therapeutic value, with many researchers and medical professionals focusing solely on CBD. However, CBDa has garnered interest in the past 10-15 years and recent studies have shown that CBDa may actually be more effective in supporting certain health issues than CBD alone.
How are actions of CBDa different from CBD?
While CBDa and CBD share similarities, there are also some important differences in terms of their bioavailability and effects, due to their chemical structures and interactions with the endocannabinoid system. CBD is known for its interaction (typically as an antagonist) with cannabinoid receptors, whereas CBDa does not interact with cannabinoid receptors but binds to 5-HT serotonin receptors. Through binding to the 5-HT receptors in the body, CBDa has the potential to play a key role in stress and mood regulation along with the ability to reduce toxin- induced nausea.
CBDa has shown greater bioavailability, so the body can metabolize the compound with less effort and in less time[1]. Because CBDa is absorbed much faster than CBD, the therapeutic effects of CBDa have a more rapid onset. For this reason, CBDa may be favorable for initial therapeutic benefits and CBD for longer-term maintenance.
4 Areas of Therapeutic Potential
The research on CBDa is in the preclinical stage, but scientists are also starting to get feedback on patient and physician case studies. There are four key areas that research already indicates promise for CBDa.
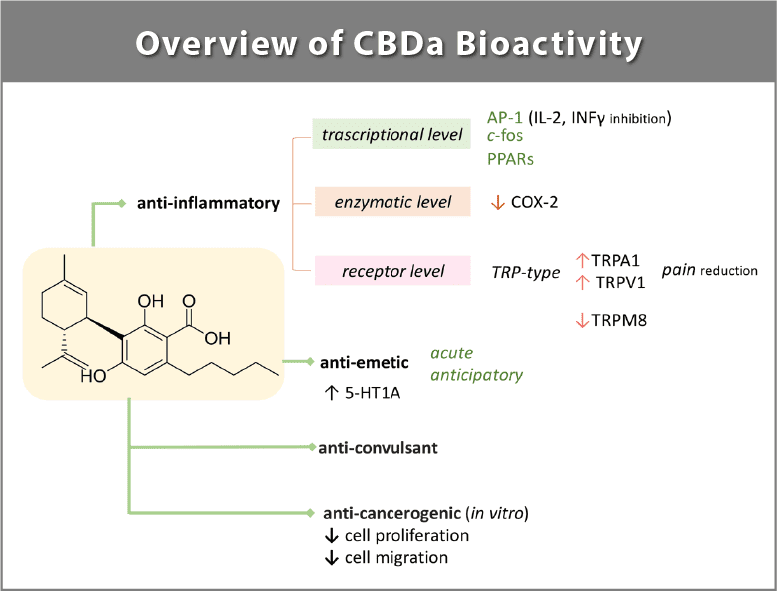
1. One of the most encouraging areas is the potential of CBDa to reduce inflammation[2,3]. Inflammation is a key factor in many chronic conditions. Researchers compared the molecular structures of CBDa with NSAIDs (nonsteroidal anti-inflammatory drugs) commonly used for inflammation and found their chemical structures to be extremely similar—both are known to inhibit COX-2 receptors[3]. Individuals looking for help with pain management may find positive results with CBDa.
2. Research shows that CBDa may be helpful for those experiencing low mood or anxiety as it binds to the body’s 5-HT1A serotonin-producing receptors, providing anxiolytic effects[4]. In fact, scientists have shown that CBDa has 100 times the affinity for the 5-HT receptors as compared to CBD[5].
3. As nausea is mediated by serotonin receptors, CBDa has also been researched for its anti-nausea properties[4,6]. A number of stressors, including radiation and chemotherapy, trigger the body to release excess serotonin, causing nausea and vomiting. By helping to reduce nausea and vomiting, CBDa may be a potential alternative to traditional anti-emetic products.
4. Recent pre-clinical research shows that CBDa may also exhibit anti-convulsive potential[7]. CBD has been clinically studied to help reduce neuron excitability, thus helping to control seizures.
Formato, et al., Cannabidiolic Acid, a Still Overlooked Bioactive Compound: An Introductory Review and Preliminary Research. Molecules. 2020; 25(11):2638.
Which should I use — CBD or CBDa?
Though CBDa shines in the areas previously mentioned, it’s not one or the other but rather the synergistic combination of CBD and CBDa that may provide the most efficacious outcomes. While they share many similar benefits, each cannabinoid also provides distinct activities and properties.
As CBDa research continues, we may discover even more applications for this powerful cannabinoid. It is important to note that research on CBDa is still in its early stages, and more research is needed to fully understand its effects and potential.
References
- Wakshlag, J. J., Schwark, W. S., Deabold, K. A., Talsma, B. N., Cital, S., Lyubimov, A., Iqbal, A., & Zakharov, A. (2020). Pharmacokinetics of cannabidiol, cannabidiolic acid, Δ9-tetrahydrocannabinol, tetrahydrocannabinolic acid and related metabolites in canine serum after dosing with three oral forms of hemp extract. Frontiers in Veterinary Science, 7.
- Rock, E. M., Limebeer, C. L., & Parker, L. A. (2018). Effect of cannabidiolic acid and Δ9-tetrahydrocannabinol on carrageenan-induced hyperalgesia and edema in a rodent model of inflammatory pain. Psychopharmacology, 235(11), 3259–3271.
- Takeda, S., Misawa, K., Yamamoto, I., & Watanabe, K. (2008). Cannabidiolic acid as a selective cyclooxygenase-2 inhibitory component in Cannabis. Drug Metabolism and Disposition, 36(9), 1917–1921.
- Pertwee, R. G., Rock, E. M., Guenther, K., Limebeer, C. L., Stevenson, L. A., Haj, C., Smoum, R., Parker, L. A., & Mechoulam, R. (2017). Cannabidiolic acid methyl ester, a stable synthetic analogue of cannabidiolic acid, can produce 5-HT1a receptor-mediated suppression of nausea and anxiety in rats. British Journal of Pharmacology, 175(1), 100–112.
- Russo, E. B. (2018). Cannabis therapeutics and the future of neurology. Frontiers in Integrative Neuroscience, 12.
- Bolognini, D., Rock, E. M., Cluny, N. L., Cascio, M. G., Limebeer, C. L., Duncan, M., Stott, C. G., Javid, F. A., Parker, L. A., & Pertwee, R. G. (2013). Cannabidiolic acid prevents vomiting in suncus murinus and nausea-induced behaviour in rats by enhancing 5-HT1a receptor activation. British Journal of Pharmacology, 168(6), 1456–1470.
- Anderson, L. L., Low, I. K., Banister, S. D., McGregor, I. S., & Arnold, J. C. (2019). Pharmacokinetics of phytocannabinoid acids and anticonvulsant effect of cannabidiolic acid in a mouse model of Dravet syndrome. Journal of Natural Products, 82(11), 3047–3055.

